
Executive summary
While COVID-19 has worsened patient waiting times across the NHS, patients with pelvic disorders have long been an under-served population experiencing unacceptable delays in care. Pelvic floor disorders are varied and can be complex, but treatment is available. However, patients, particularly those requiring surgery, can wait years from presentation before receiving the treatment they need. Patients with more than one area of the pelvis (compartment) affected may wait even longer while they see multiple specialists to treat their disorder. And all the time they are living with the profound impact of their condition, with some afraid even to leave the house.
WE MUST CHANGE THIS SITUATION AND MAKE SURE THAT IN THE FUTURE, PATIENTS RECEIVE THE CARE THEY NEED IN A TIMELY MANNER.
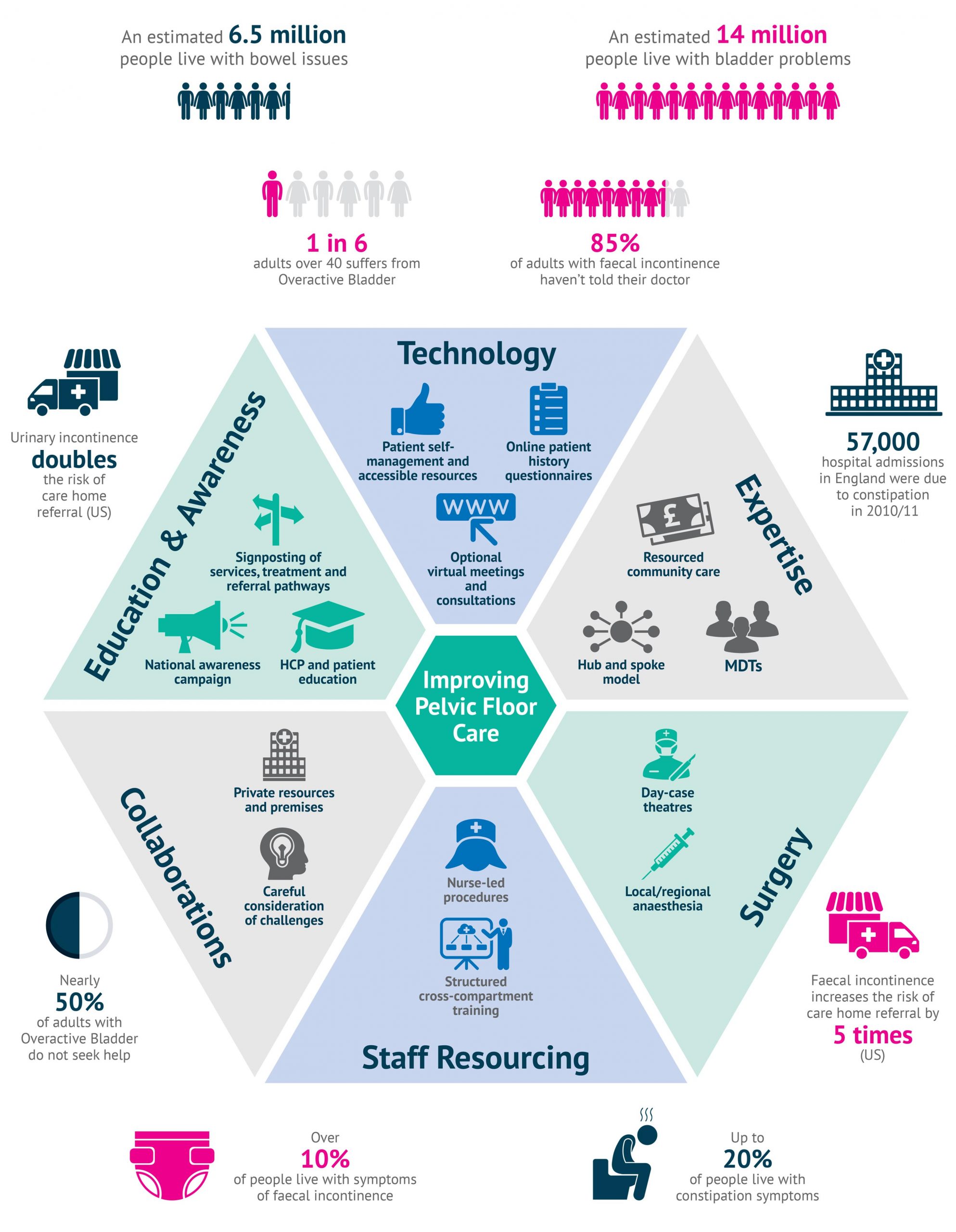
WE PROPOSE CHANGES IN SIX KEY AREAS:
- Empowering and educating patients and beyond
- Making use of technology
- Integrating expertise
- Looking again at surgical procedures
- Making the most of our teams
- Considering collaborations
Each area is addressed with its own chapter, but a brief summary is provided below.
A national, well-funded campaign is needed to raise awareness of the options for treatment
Empowering and educating patients and beyond
The taboo surrounding pelvic floor disorders is a major barrier to treatment; also, some patients do not realise that treatments may be available. A national, well-funded campaign is needed to break down this taboo and raise awareness of the options for treatment; it should also offer education on maintenance of bladder and bowel health.
Patients must be encouraged and empowered to present for treatment and to refer themselves if necessary – this requires the provision of adequate and accessible information, support and services. Early intervention can address the problem before it progresses to the stage that invasive therapies are required: it is important that patients are aware that conservative (non-surgical) interventions exist at an early stage of their disorder, as fear of invasive procedures can be another barrier.
It can take years for patients to present or to reach the right specialist. More needs to be done to ensure that when they do seek help from a healthcare professional (HCP), whatever the stage of their journey, they are taken seriously and are signposted to someone who can help them. Improved education for midwives and HCPs in primary care, particularly GPs and nurses, can help ensure patients receive the support and understanding they need when they present and that they are able to access the right specialist services for their condition.
Making use of technology
COVID-19 has accelerated the adoption of digital platforms to communicate with patients and colleagues. People living with pelvic floor disorders face barriers to attending in-person appointments, particularly in relation to travelling. A choice of telemedicine and in-person consultations is recommended based on patient and physician needs, such as for physical examination. We must make particular efforts to make consultation and treatment accessible to hard-to-reach communities. Online questionnaires allow accurate patient histories to be collected in advance, making clinics more efficient.
Accessibility of and sign-posting to high-quality supportive patient information and resources is important. Patients may benefit from the use of apps or websites to take ownership of their condition and find additional support; however, as it stands, online resources are often challenging for patients to find; further, they may not know which sources are evidence-based, and not all patients have access to the internet.
Technology can also improve clinicians’ daily work experience and education. Virtual multidisciplinary team (MDT) meetings have increased attendance, allowing participants to join from different sites, as well as allowing patients from a local MDT to be discussed with the regional teams. Technology allows for improved access to HCP education and e-learning is increasingly accepted following the tectonic shifts brought about by COVID-19.
Many pelvic floor problems do not require hospital care. Seeing patients in their own home can be beneficial
Integrating expertise
There is an inequality of access to pelvic floor services across the UK, with expertise dispersed around the country and funding and manpower shortages in community care in some areas. The importance of community continence care cannot be overstated, and adequate funding is essential. Many pelvic floor problems can be dealt with efficiently in the community without requiring the resources associated with hospital visits.
In order to better identify patients who truly need hospital care along with those whose condition can be managed in the community, triaging systems that are already used in some centres can help to prioritise patients who require more specialist support.
A hub-and-spoke approach could make the most of available expertise and this should be tailored by region accepting that some will have ‘spokes’ with specialist expertise, capacity or facilities. This approach will ensure the experts of the future are adequately trained, providing centres with a high concentration of cases and expertise for trainees to learn from.
Such approaches should tie in with full UK adoption of regional MDT working. The Pelvic Floor Society offers a system of voluntary accreditation, making a standardised approach and high standards achievable across the country.
Looking again at surgical procedures
A key road-block for surgical procedures is the long waiting time for theatre availability – worsened by the COVID-19 crisis. However, not all surgery needs to take place in the operating theatre under general anaesthesia. Transitioning appropriate procedures to local or regional anaesthetic in clean rooms or day-case theatres will free up space and help reduce waiting times.
Some centres are already making this change for specific procedures e.g. sacral neuromodulation or Botox injections. Concomitant changes in facilities and training require investment to ensure safety and quality.
Making the most of our teams
Trained nurses and other AHPs, such as physiotherapists, can conduct some protocol-driven procedures to free up specialists for other work. Botox administration and sacral neuromodulation (SNM) are nurse-led in some centres, resulting in reduced waiting times.
MDTs enable regions to make the most of expertise and availability. NICE guidelines recommend both local and regional MDTs, with local meetings reviewing treatments for primary stress urinary incontinence, overactive bladder or primary prolapse, and regional meetings to cover multi-compartmental prolapse and mesh-related problems.
Maintaining a sufficient workforce to meet the needs of patients in the future is an important consideration, particularly given current shortages. While colorectal, urology and urogynaecology specialists may have a primary calling to their own speciality, we should aspire to train future ‘pelvic floor’ surgeons (and nurse and allied specialists), to firmly consign fragmented and poorly coordinated treatment between pelvic compartments to the past. This is important not least because ignorance of multicompartmental problems can lead to surgery where the opportunity to address two problems at the same time is lost – or, worse still, one problem is made worse by surgery on another. Notably, all stages of medical education, from undergraduate to professional development, should include sufficient emphasis on pelvic floor and continence to ensure that this public health challenge is recognised and addressed.
Collaboration with private institutions and premises could help to address specific capacity challenges
Considering collaborations
With continually growing waiting lists and the ongoing problem of COVID-19, collaborating with private institutions and premises could help to address specific capacity challenges. This is not a new approach: the first wave of COVID-19 made NHS use of private resources necessary, and the experiences gained during this period can offer valuable insights for tackling resourcing challenges moving forward.
Particularly for day cases, the use of private facilities, such as treatment centres, could help to further free up space and reduce the backlog. Potential challenges must be carefully considered, including staff availability, patient selection, quality assurance and follow-up care.
PELVIC FLOOR CONDITIONS: THE BIG PICTURE